Blog

Preventing Falls at Home for Children

Preventing falls at home is essential for keeping children safe as they explore their surroundings. Using stationary walkers and playpens can provide secure play areas, while installing safety gates helps block access to stairs and other risky spots. It is important to keep stairs clear of clutter and avoid placing toys or tempting items on top of furniture where children might climb. Despite precautions, falls can still occur and may lead to foot injuries, such as sprains, fractures, or bruises. A podiatrist can assess the extent of these injuries, provide proper treatment, and guide recovery with supportive footwear. If your child has balance issues or sustained a foot or ankle injury from falling, it is suggested that you confer with a podiatrist who can treat various injuries, and guide you effective fall prevention techniques.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with one of our doctors from Favor Foot Ankle Leg & Wound Center. Our doctors will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in South Amboy, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
Plantar Fasciitis and Podiatry Care
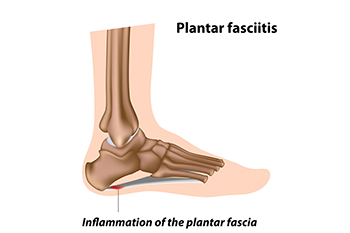
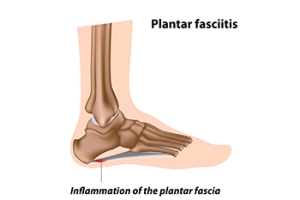
Plantar fasciitis is caused by inflammation of the plantar fascia, the thick band of tissue that runs along the bottom of the foot and supports the arch. This condition often leads to sharp heel pain, especially with the first steps in the morning or after long periods of rest. Risk factors include prolonged standing, flat feet, high arches, obesity, and wearing footwear that lacks proper support. Symptoms include aching, stiffness, or a burning sensation in the heel. If left untreated, the pain can become chronic and interfere with daily activities. A podiatrist can diagnose plantar fasciitis, provide targeted stretching exercises, and offer custom orthotics or treatments to relieve pain and promote healing. If you have heel pain, it is suggested that you consult a podiatrist who can accurately diagnose and treat the condition.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our doctors from Favor Foot Ankle Leg & Wound Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in South Amboy, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Stretching Exercises for Achilles Tendonitis
Achilles tendonitis involves inflammation in the tendon that connects the calf muscles to the heel bone, often the result of overuse or repetitive strain. A podiatrist may recommend specific stretching and strengthening exercises to help relieve tension, improve mobility, and support long-term recovery. Calf stretches, such as the runner’s stretch or toe-to-wall stretch, can reduce tightness and ease strain on the Achilles tendon. Another useful stretch is the heel drop, which involves slowly lowering the heel below a step to gently lengthen the tendon. Once stretching is tolerated, strengthening exercises like seated heel raises and controlled resistance band movements may be introduced to reduce the likelihood of reinjury. These exercises aim to support the structures surrounding the Achilles tendon and protect it during activity. A podiatrist can evaluate the severity of the condition and determine if additional support, like custom orthotics or surgery, is needed. If you are experiencing Achilles tendon pain, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment, which may include targeted exercises.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our doctors of Favor Foot Ankle Leg & Wound Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in South Amboy, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
When a Cut on the Foot Should Be Left Open

Not every foot cut needs to be covered all the time. In some cases, letting a minor wound breathe can help it to heal faster. Small, clean cuts without signs of infection may benefit from short periods of air exposure, which can dry the surface and support natural healing. However, this only applies when the area is protected from dirt, pressure, and further injury. Cuts in moist areas or places that rub against shoes should usually stay covered to avoid irritation. If a wound is deep, bleeding heavily or shows redness, swelling, or drainage, it should be kept clean, protected, and watched closely. People with diabetes or poor circulation should always cover foot cuts to reduce the risk of infection. If a cut on your foot does not heal or becomes painful, it is suggested you see a podiatrist for appropriate treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our doctors from Favor Foot Ankle Leg & Wound Center. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in South Amboy, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Types and Symptoms of Toenail Fungus

Toenail fungus, also called onychomycosis, usually occurs when tiny cracks in the nail or surrounding skin allow fungi to enter and grow. The most common types of toenail fungus include infections that start at the tip of the nail and move inward, infections that cause white patches across the surface, and infections that begin at the base of the nail and spread toward the tip. Symptoms include nails becoming thick, brittle, discolored, crumbly, or giving off an unpleasant odor. Risk factors for toenail fungus include older age, diabetes, poor circulation, and walking barefoot in public places like pool areas and gym locker rooms. A podiatrist can diagnose the infection by examining the infected toenail and testing a small sample, if needed. Treatment options generally start with antifungal medication, but in severe cases, surgery may be needed to remove the infected nail. If you believe you have a fungal toenail infection, it is suggested that you make an immediate appointment with a podiatrist for appropriate treatment.
For more information about treatment, contact one of our doctors of Favor Foot Ankle Leg & Wound Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our office located in South Amboy, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.